Schizophrenia and Psychosis
What Is Schizophrenia?
Schizophrenia, coined by Eugen Bleuler in 1908, is a prototypical psychiatric disorder wherein the afflicted individual could have delusional beliefs, and abnormal perceptions like illusions and hallucinations; with or without disturbances in thought and behavior.
Of Greek origin, the word schizophrenia originates from a “schism” or split between thoughts, emotion and behavior such that the three become incongruent and disconnected. That is when one is believed to have lost rationality, judgment and the connection with reality. People with schizophrenia are believed to live in an illusionary, delusional world of their own; that is indecipherable to others around them. Schizophrenia is known to affect 1% of the population in general and usually has a better prognostic outcome if detected well in time.
Schizophrenia: Fact 1
Schizophrenia is usually sseen in the late teen years to the early thirties and tends to appear earlier in males (late adolescence – early twenties) than females (early twenties – early thirties).
Schizophrenia: Fact 2
The first episode of psychosis or unrealistic behavior does not qualify as schizophrenia. Only when it has persisted for a period of time and is unrelenting, do we diagnose schizophrenia.
Schizophrenia: Fact 3
Psychosis and schizophrenia are never sudden even though it appears so. Subtle changes in thinking, emotion and behavior are gradual and consistent; they’re just not noticed so easily.
Schizophrenia: Fact 4
Schizophrenia can have a combination of a few or many categories of positive symptoms, mood abnormalities, withdrawal or negative signs as well as cognitive or neurological disturbances.
Schizophrenia: Fact 5
Genetics are strongly proposed in schizophrenia and yet there is no guarantee that if a parent has it then the child will have it. Also, those without family history may still be affected at times.
Schizophrenia: Fact 6
Schizophrenia may not be “curable” but symptoms can be controlled with medication, lifestyle modification, stress control and a supporting environment. It takes effort but this is attainable.
Is Schizophrenia Serious?
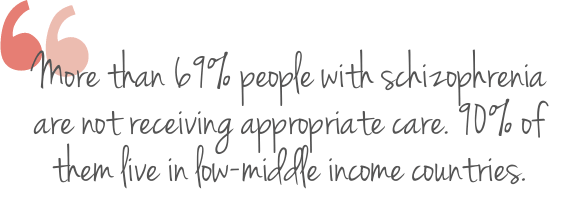
In general, one out of every 100 individuals have schizophrenia. That’s not a trivial number. And the degree to which this affects a person in terms of lack of ability for self-care, incapacity to work or fend for themselves, and consistent need for supervision in serious cases; makes it a burdensome illness.
Although worldwide the prevalence doesn’t seem as much, the burden it poses globally is immense. A large number of people with schizophrenia have other psychiatric and physical illnesses. Data emphasizes that such people have a 20% reduction in life expectancy; and nearly 40% of deaths in schizophrenia could be attributable to suicide. It may appear to be more common in men, but it’s also possible that lesser women report it. Schizophrenia is a serious mental illness that reduces the capacity for a wholesome and fulfilling life.
Why Does One Develop Schizophrenia?
Biological theories have long been proposed to explain schizophrenia; with specific brain regions showing structural and functional aberrations in neural circuitry and chemicals (predominantly dopamine, serotonin, GABA and glutamate). The golden question still remains, why does this occur in some people and not others?
Neurodevelopmental theories emphasize in utero (prior to birth) trauma to the brain (maternal malnutrition, influenzas, cannabis use, hypertension and other prenatal complications) that affect the neural connections prior to birth itself. The most accepted explanation these days is a genetic vulnerability, which superadded with significant emotional stress that is beyond an individual’s coping capacity, leads to breakdown in the defense circuitry leading to an expression of schizophrenia.
Generally, people who are insecure, unsure, indecisive, over perfectionistic, hyper sensitive to criticism and overly critical, tend to develop paranoid tendencies and could get delusional more than others. Stressors that predispose to psychotic behavior are subjective. Those with immature coping mechanisms tend to react adversely to stressful situations and could have a psychotic breakdown more readily. With all research ongoing, we still know little and need to understand schizophrenia better because it is debilitating. For the patient and the family.
Are There Types of Schizophrenia?
Schizophrenia is believed to exist on a spectrum of severity and described with different symptoms. Paranoid schizophrenia is the commonest, with delusions, hallucinations, muddled words, trouble concentrating, impulsivity, emotional instability and often inability to reveal emotions. The disorganized variety is free of delusions and hallucinations; but exhibits greater inefficiency in thinking with abnormal or odd behavior; such that makes everyday activities could get impossible to accomplish.
Catatonic schizophrenia is explained by immobility; a stupor like condition wherein one does not communicate at all, and simply imitates what another person does. Sometimes when a person with schizophrenia no longer has active troubling symptoms, there may still be some mild disturbances which bring one a diagnosis of residual schizophrenia. Symptoms could present early on in life where childhood schizophrenia is the case.
What Are the Symptoms and Signs of Schizophrenia?
Schizophrenia is categorized as the prototype of psychotic disorders that enable one to lose touch with reality. Although its presentation is diverse, some common symptoms of psychosis define its diagnosis. These could be positive negative, cognitive and behavioral symptoms.
Hallucinations (seeing, hearing or generally sensing things that aren’t really there); delusions (a false but firm belief that persists in spite of all evidence to the contrary), and formal thought disorders (losing the train of thought or speaking indecipherable concepts); are called positive symptoms in schizophrenia. They imply that something is going on which is clearly not normal. Negative symptoms, involve a gradual and enduring loss in thought, emotion and action and include slowness and paucity of speech, anhedonia or inability to feel any emotion; and abulia (a lack of motivation for anything). Negative symptoms may also be called post schizophrenic depression as they simulate emotional features seen in major depression.
Some symptoms might be specific to the variety of schizophrenia. Any of these in you or someone you know, should raise your antennae and coax you to seek professional help.
Positive Symptoms
- Loss of a sense of shared reality
- Distorted experience of the world
- Hearing or seeing imaginary things
- Believing things that are not true
- Unusual thinking and odd speech
Negative Symptoms
- Decreased motivation for things
- Inability to plan or sustain a plan
- Reduced speech and expressivity
- Inability to feel pleasure anymore
- Difficulty in displaying emotions
Cognitive Symptoms
- Difficulty processing information
- Confusion and memory lapses
- The mind going blank or empty
- Irrational and illogical thinking
- Losing the connect in conversation
Emotional Symptoms
- Fearfulness, feeling extremely afraid
- Extreme paranoia or suspiciousness
- Sense of being referred to all the time
- Irritability, frustration or outbursts
- Inability to express or relate to people
How Does Family Support Play a Role?
It’s really important for family to understand symptoms, treatment options, and the course of recovery for a relative with schizophrenia. Family education on the concept, presentation and treatment of the illness (also known as psychoeducation) is known to enhance patient support and influence more positive outcomes because family support is protective and restorative both.
Family Must Remember
- This is not a cry for attention
- What patients feel, is very real
- Acknowledge how they feel
- Don’t react back emotionally
- Assess for safety (self & others)
- Be respectful and supportive
- Encourage professional help
Differential Diagnosis
- Substance-induced psychoses
- Mood disorders with psychoses
- Delusional disorder
- Paranoid personality disorder
- Schizotypal personality disorder
- Pervasive developmental disorder
- Psychosis due to neurological cause
Schizophrenia Management By Dr Shefali Batra
We initiate a detailed discussion with the patient (as well as family or loved ones where possible) and chalk out a treatment plan that embraces combined goals, preferences and pace of self-work. As a psychiatrist and psychotherapist practicing distinctive therapies, Dr Shefali guides you through cognitive, mindfulness and neurobehavioral milestones to help you think, feel and behave more meaningfully.
Medication helps correct the neurochemical imbalance in all psychotic disorders including schizophrenia. These include oral second-generation antipsychotic (SGA) medicines with a better side effect profile; as well as other medication if needed for concomitant anxiety, depression or sleeplessness. Schizophrenia is challenging because symptoms tend to persist even in the absence of severe psychotic breakdown.
Cognitive behavioral therapy (CBT) can complement medication management and evidence has shown its effectiveness in reducing positive and negative symptoms, softening delusions, improving insight, enhancing medication compliance, and lessening aggression. CBT is safe, and caregivers can help with homework exercises too. The aim is to help the normalize and make sense of unrealistic psychotic experiences, and to reduce the associated distress and impact on everyday life. The effect of CBT is slow but the more consistent one is; therapy holds better impact.
Dr Shefali Batra was interviewed by VERVE Magazine on Demystifying Mental Health. She explained the applicability of different therapies in various psychological conditions and how they help.


References
Hany, M., Rehman, B., Azhar, Y., et al. (2021). Schizophrenia. StatPearls. Treasure Island (FL): StatPearls Publishing
Rathod, S., Phiri, P., & Kingdon, D. (2010). Cognitive behavioral therapy for schizophrenia. The Psychiatric clinics of North America, 33(3), 527–536.
Messias, E. L., Chen, C. Y., & Eaton, W. W. (2007). Epidemiology of schizophrenia: review of findings and myths. The Psychiatric clinics of North America, 30(3), 323–338.
Related topics
- Mood Disorders
- Lifestyle Disorders
- Childhood Depression
- Cognitive Behavioral Therapy
- Acceptance Commitment Therapy
Latest Posts
7 Reasons Why You Should Seek Therapy

5 Time Wasters You Need to Overcome
5 Signs you have no work life balance
Work and Life: What is the right balance?